Although many people who contract COVID-19 have either no symptoms or mild ones, some require intensive care for pneumonia with acute respiratory distress syndrome. Risk factors for severe disease include older age, heart disease, cancer and diabetes, but these characteristics alone are not sufficient to predict which patients will become the sickest. Measuring levels of biomarkers in the blood could help, but these tests are often slow, complicated or expensive. For more effective triage of COVID-19 patients at hospitals, researchers aimed to develop an easy-to-use method that could quickly and cost-effectively predict COVID-19 severity.
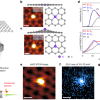
To measure changes in blood biochemistry that occur with severe COVID-19, the researchers chose attenuated total reflectance Fourier transform infrared (ATR-FT-IR) spectroscopy, which has been tested previously as a COVID-19 diagnostic tool. Two regions of spectra from 128 patient plasma samples showed small but observable differences between those with severe and non-severe COVID-19. Using these data together with clinical information about patients, the researchers developed a statistical model to predict COVID-19 severity. They found that the best predictor was whether the patient had diabetes, followed by the two regions in the FT-IR spectra. Adding the FT-IR data to the model improved the sensitivity for detecting severe disease in a different set of 30 patients from 41.2 % to 94.1 %, but reduced the specificity from 84.6 % to 69.2 %, compared with the clinical factors alone. This means that the new test was more likely to identify severe cases, but it also had a higher rate of false positives, than the clinical data alone. Although the strategy needs to be tested in larger numbers of patients, it shows promise as a rapid, simple and economic triaging test for hospitals, the researchers say.