More than 13 million pain-blocking epidural procedures are performed every year in the United States. Although epidurals are generally regarded as safe, there are complications in up to 10% of cases, in which the needles are inserted too far or placed in the wrong tissue.
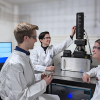
A team of researchers from Massachusetts Institute of Technology (MIT) and Massachusetts General Hospital (MGH) hopes to improve those numbers with a new sensor using Raman spectroscopy that can be embedded into an epidural needle, helping anaesthesia doctors guide the needle to the correct location.
Currently, anesthesiologists must guide a four- to six-inch needle through multiple layers of tissue to reach the epidural space surrounding the spinal cord. They know when the needle has reached the right spot based on how the tissue’s resistance changes. However, some patients’ tissues vary from the usual pattern, which can make it more difficult to determine whether the needle is in the right place.
“The needle is placed essentially blindly”, says T. Anthony Anderson, an anaesthesiologist at MGH and an assistant professor at Harvard Medical School. “The needle can go too far or into the wrong tissue, which means the patient doesn’t get the positive effect that you want or is injured.”
In most cases, these complications lead to reduced effectiveness of the pain-killing drug, or an excruciating post-procedure headache. In rare cases in which the needle goes too far or into a blood vessel, a stroke or spinal cord injury can occur.
To improve the accuracy of epidural needle placement, Anderson teamed up with researchers at MIT’s Laser Biomedical Research Center, headed by Peter So, a professor of mechanical engineering and biological engineering. So and MIT research scientist Jeon Woong Kang designed and tested several types of optical sensors that could be placed at the tip of an epidural needle and determined that the best used Raman spectroscopy. The researchers measured the concentrations of albumin, actin, collagen, triolein and phosphatidylcholine using Raman spectroscopy and were able to accurately identify different tissue layers.
This sensor, which the researchers described in Anesthesiology, provides immediate feedback telling the anaesthesiologist which tissue the needle is in. As an epidural needle is inserted, it passes through five layers—skin, fat, supraspinous ligament, interspinous ligament and ligamentum flavum—before reaching the epidural space, which is the target. Beyond that space lies the dura mater, a stiff membrane that surrounds the spinal cord and cerebrospinal fluid.
“The sensor is continuously measuring Raman spectroscopy signals, which tells you the chemical composition of the tissue. From the chemical composition you can identify all tissue layers, from skin to spinal cord”, Kang says.
The team found that Raman spectroscopy could distinguish each of the eight tissue layers around the epidural space with 100% accuracy. Two other techniques that they tested, fluorescence and reflectance spectroscopy, could distinguish some layers but not all eight.
The researchers have tested the sensor in pig tissue and now plan to do further animal studies before testing it in human patients. They also plan to reduce the diameter of the sensor slightly, from 2 mm, which is too large to fit in the most commonly used epidural needles, to 0.5 mm.